Question:
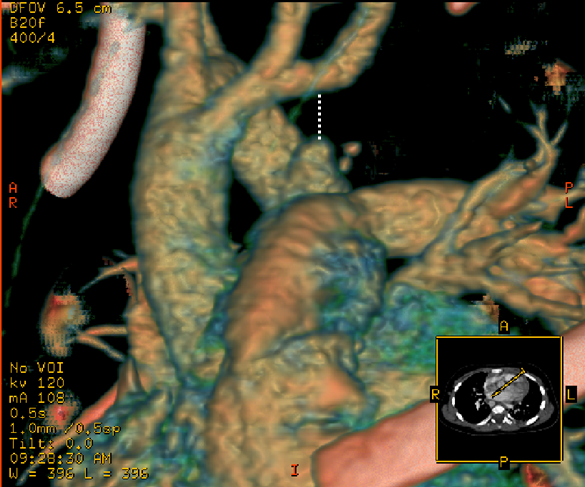
13-year old patient who underwent
repair of coarctation of aorta earlier that day has two arterial lines, right
radial & left femoral. According to the reading on the monitor, apparent
peak to peak pressure gradient across the coarctation repair site is 37 mmHg.
Question: Based on the traces in
each arterial line, is the pressure gradient higher than, lower than or equal
to 37 mmHg? Why?
Answer:
The peak to peak pressure gradient is lower than 37 mmHg.
Right radial arterial line trace has a “whip”, “fling” or “standing wave” (or
as Ashish puts it in sophisticated terms…”distal pulse amplication”) that
artificially increases the systolic pressure. Left femoral arterial line has a
more rounded peak which is characteristic of a more central arterial line
trace. Since the fling or standing wave overestimates the systolic pressure in
radial arterial line, gradient of overestimated. Real systolic pressure in
right radial arterial line is unfortunately not possible due to technical
limitations.
Systolic and diastolic arterial blood pressures are higher and lower, respectively, in radial arteries than in the aorta. This phenomenon is known as distal pulse amplification and is due to the characteristics of the vascular tree. Briefly, a pulse waveform entering the aorta is exposed to a sudden impedance change at the capillary level, resulting in a large increment in resistance and producing reflected pulse waveforms. Those waves are added to the following ones, producing higher peaks than the original aortic systolic peak at different distances from the aortic origin. This distal pulse amplification is always present when peripheral vascular resistance is high.
Reference: Peripheral arterial blood pressure monitoring adequately tracks central arterial blood pressure in critically ill patients: an observational study. Mariano Alejandro Mignini, Enrique Piacentini and Arnaldo Dubin. Critical Care 2006;10:R43.