Called to evaluate a term, 1-day old baby for “bradycardia”
(~90 bpm). EKG is given. (Clue: V1 rhythm strip provides best wave forms to
evaluate).
Question: (i) What is the cause of this relative “bradycardia” in this baby? (ii) Explain why AV block is not the primary diagnosis?
Answer:
(i) Cause for “Bradycardia” is non-conducted atrial ectopies.
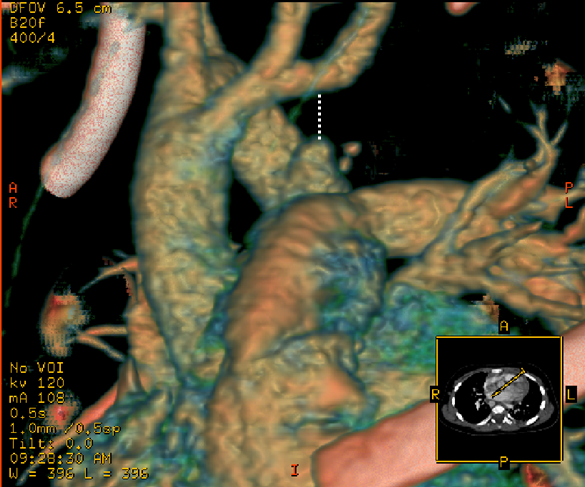
There is an atrial ectopy after each QRS (arrows in the figure below) that is not conducted. This
is a “physiologic” block because atrial ectopy is too early for the AV node to
conduct. Further, the atrial ectopy depolarizes and resets the SA node (as
opposed to ventricular ectopy that usually does not). Therefore, SA node fires
somewhat later than usual after an atrial ectopy leading to overall slowing of
heart rate.
(ii) AV block is not the primary diagnosis because the "block" is secondary to the early timing of the atrial ectopy. AV block is a physiologic event in this situation - not a block at all.
(ii) AV block is not the primary diagnosis because the "block" is secondary to the early timing of the atrial ectopy. AV block is a physiologic event in this situation - not a block at all.
(Unfortunately, the T waves are flat leading to some
confusion in recognizing the atrial ectopies).
(Click on the image to enlarge) Arrows indicate "blocked atrial ectopies"